Equine grass sickeness is a somewhat mysterious disease that is often fatal. It strikes down healthy young horses as they graze. Early clinical signs resemble those of mild colic. As the disease progresses, horses show patchy sweating, muscle tremors, elevated heart rate, difficulty in swallowing, and sluggish or absent gut motility.

Blood tests to diagnose Equine Grass Sickness
Although the acute and subacute types of Equine Grass Sickness are almost always fatal regardless of treatment, horses with chronic EGS may survive if they can be persuaded to eat high-energy concentrated feeds..
Acute cases almost always result in the death of the horse within one to five days after signs appear. Horses with subacute EGS may survive for a few weeks, showing progressive weight loss before finally succumbing to the disease.
A chronic, low-level type of EGS is characterized by the same signs, but can be treated by intensive veterinary care. Some horses survive chronic EGS but they usually lose a great deal of weight.
What treatments for Equine Grass Sickness are available?
Although the acute and subacute types are almost always fatal regardless of treatment, horses with chronic EGS may survive if they can be persuaded to eat high-energy concentrated feeds. Intravenous fluid therapy is used to prevent dehydration. Cisapride, a human medication that increases gut activity, has been helpful in some cases.
What is the outlook for horses with EGS?
Horses with chronic EGS lose hundreds of pounds of body weight due to a progressive degeneration of nerves that control gut function. As the disease passes, they start to regain condition and can usually return to work or training over a period of several months.
What causes EGS?
Years of study and speculation followed the first description of this disease early in the twentieth century. Several theories were advanced as to the cause, including one that focused strong suspicion on botulin toxicity. The most recent studies have confirmed a definite link to Clostridium botulinum type C organisms, with affected horses having lower levels of antibodies to C. botulinum type C and its toxins than those found in control animals.
However, the soil-dwelling botulin organisms are widespread and are presumably encountered many times by grazing horses. The question remains as to whysome horses develop grass sickness while others do not.
What are the major risk factors?
A study at the University of Liverpool has identified factors associated with cases of EGS:
- Some premises have a high incidence of EGS, while other nearby areas are unaffected.
- More cases are found in areas with acidic loam and sand soils; fewer cases occur where the soil is composed of clay or chalk.
- Risk is increased with soil disturbance such as that caused by mechanical manure removal.
- Risk is lowered when fields are also grazed by ruminants, but the presence of domestic poultry raises the risk.
- Although foals seem to be protected, young horses (up to about five years old) are the most common victims, possibly because they have not had enough exposure to bacteria to build a protective level of antibodies.
- Animals that are under increased stress due to castration, breaking, or shipping are more susceptible.
- Risk is higher in horses that have had any change in feeding schedule such as increased or decreased amount of concentrate, change in concentrate/forage ratio, turnout after a period of stalling, or grazing a different pasture.
- Recent deworming with an ivermectin product seems to be linked to increased risk, although scientists are not sure how to interpret this finding. Owners should not see this link as a recommendation to stop deworming treatments.
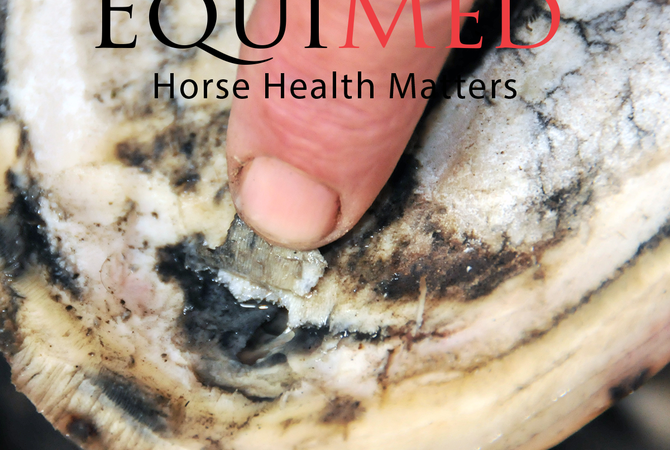
Until recently, Equine grass sickness (EGS) has presented a diagnostic challenge. The best way to confirm the diagnosis is by finding characteristic signs in biopsies of the small intestine.
However this entails general anaesthesia and abdominal surgery, making it expensive. Other tests have been used to try to throw light on the diagnosis, such as the response to phenylephrine eye drops.
The latest issue of Equine Science Update reports that blood tests may help narrow down the diagnosis in some cases of suspected grass sickness.
Horses with equine grass sickness may show signs of systemic inflammation. One way of identifying this is to look for acute phase proteins (APPs) in the blood. As their name suggests, these are proteins that increase in concentration in the blood in the early stages of an inflammatory response..
Researchers at Liphook Equine Hospital and the Royal (Dick) Vet College tested serum samples from 40 horses with EGS and compared them with 20 healthy horses, including those grazing the same pasture, and eight horses with colic due to causes other than EGS.
They found a marked increase in serum amyloid A (SAA) and fibrinogen in horses with EGS, and in horses with inflammatory colic, such as peritonitis, enteritis or colitis, compared with healthy horses, co-grazers and horses with colic due to non-inflammatory causes, such as intestinal obstruction.
There was no significant difference in SAA levels between horses with EGS and those with an inflammatory colic.
Interestingly they also found concentrations of another APP, Activin A, were significantly increased in both EGS cases and co-grazing horses. They suggest that this might indicate the presence of sub-clinical disease in the co-grazers.
In a report of the work which was published in the Veterinary Record, Victoria Copas and co-workers suggest that a marked increase in fibrinogen and SAA concentrations may help differentiate cases of EGS from other causes of abdominal pain (such as simple colon obstructions or intestinal strangulations) when considered in conjunction with signalment, historical data, clinical findings and results of other ancillary diagnostic tests.
However, they emphasise that doing so would not help differentiate between EGS and other inflammatory abdominal conditions – such as peritonitis or enteritis