A team of cell biologists has discovered why treatment of mesenchymal stem cells (MSCs) with the mycotoxin cytochalasin D directs them to mature into bone cells (osteoblasts) rather than into fat cells (adipocytes), a finding that might prove useful in the development of treatments for bone loss. Although the research has been done using mice as subjects, this research has implications for both horses and humans.

New hope for bone injury treatment in horses
A team of cell biologists has discovered why treatment of mesenchymal stem cells with the mycotoxin cytochalasin D directs them to mature into bone cells, and while mice have been used as subjects, this research has implications for both horses and humans.
Mesenchymal stem cells, or MSCs, are multipotent stromal cells that can differentiate into a variety of cell types, including: osteoblasts, chondrocytes, myocytes, and adipocytes.
Cytochalasin D is a cell-permeable and potent inhibitor of actin polymerization. It disrupts actin microfilaments and activates the p53-dependent pathways causing arrest of the cell cycle at the G1-S transition. It is thought to bind to F-actin polymer and prevent polymerization of actin monomers.
Investigators at the University of North Carolina School of Medicine (Chapel Hill, USA) reported in the October 2015 issue of the journal Stem Cells that cytochalasin D treatment caused transfer of G-actin into the nucleus.
The continued presence of rod-like structures of actin in the nucleus was associated with induction of robust expression of the osteogenic (bone forming) genes osterix and osteocalcin in a Runx2 (Runt-related transcription factor 2)-dependent manner, and led to acquisition of an osteogenic phenotype.
Adipogenic (fat forming) differentiation also occurred, but to a lesser degree. Injection of cytochalasin D into the tibial marrow space of live mice resulted in abundant bone formation within the space of one week.
The RUNX2 gene is a member of the RUNX family of transcription factors and encodes a nuclear protein with a Runt DNA-binding domain. This protein is essential for osteoblastic differentiation and skeletal morphogenesis and acts as a scaffold for nucleic acids and regulatory factors involved in skeletal gene expression.
The findings obtained during this study suggested that actin inside the nucleus caused Yes-associated protein (YAP) to leave the nucleus, and that it was the activity of YAP within the nucleus that had been inhibiting the Runx2 initiation of bone formation.
âAmazingly, we found that the actin forms an architecture inside the nucleus and turns on the bone-making genetic program,â said senior author Dr. Janet Rubin, professor of medicine at the University of North Carolina School of Medicine.
âIf we destroy the cytoskeleton but do not allow the actin to enter the nucleus, the little bits of actin just sit in the cytoplasm, and the stem cells do not become bone cells. What we have found could become an amazing way to jump-start local bone formation. However, this will not address osteoporosis, which involves bone loss throughout the skeleton.â
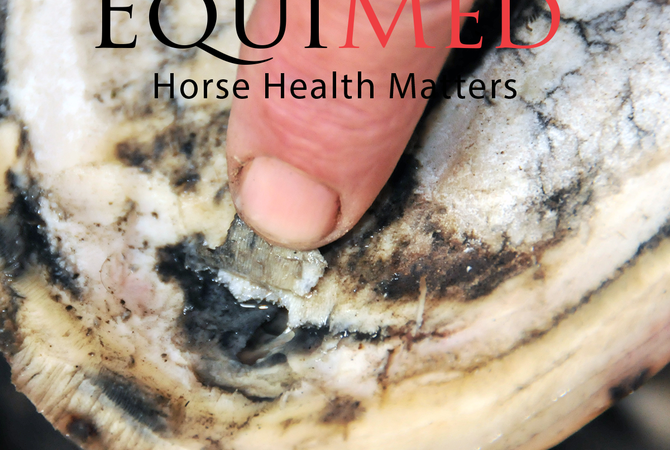
âThe bone forms quickly,â said Dr. Rubin. âThe data and images are so clear; you do not have to be a bone biologist to see what cytochalasin D does in one week in a mouse.â Although this process will not affect osteoporosis, the implications for healing of fractured or broken bones may prove to be a major step in saving horses with bone limb injuries.